Articles
The Gut-Brain Axis: An Emerging Key to Brain Health
Published: April 15, 2025
Author: Achilles Neurology Clinic
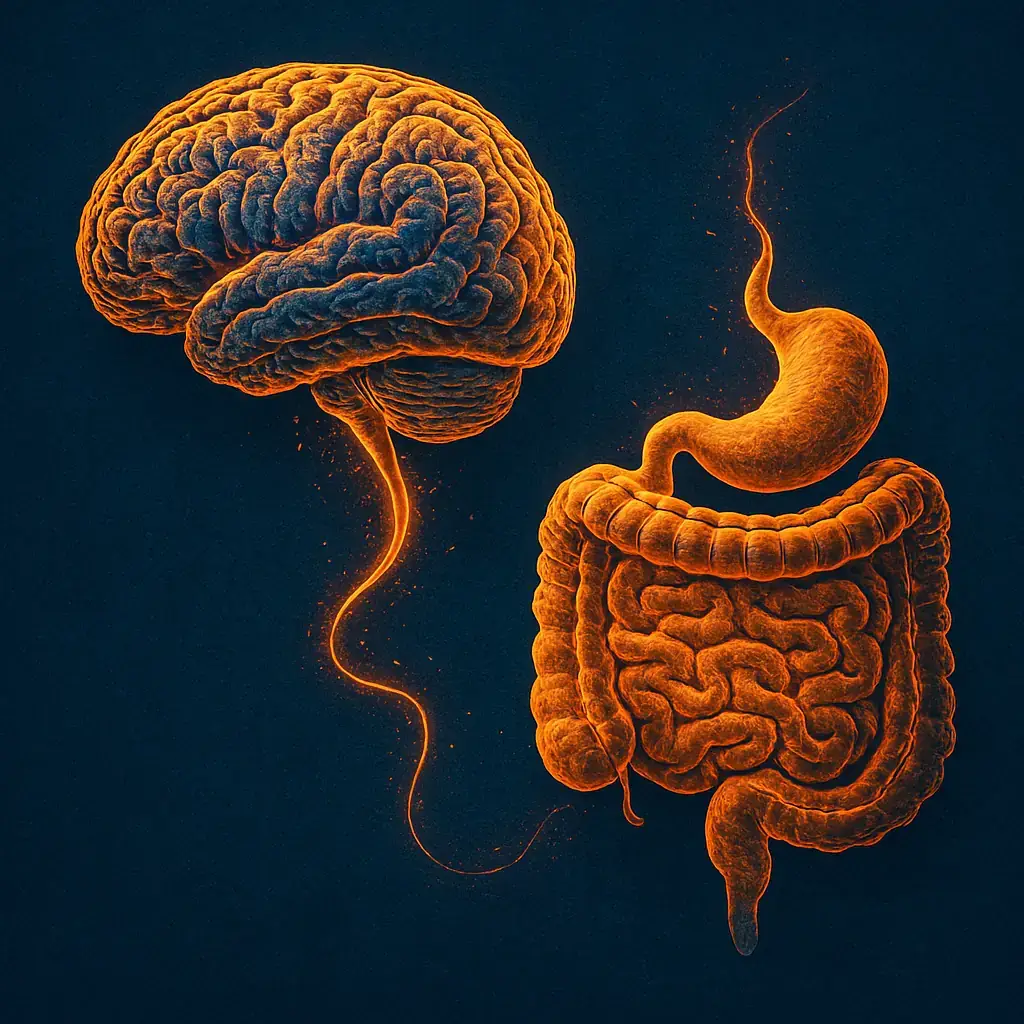
Ever had "butterflies" in your stomach when you were nervous, or felt a "gut-wrenching" emotion? These common sayings hint at a fascinating truth: our gut and brain are in constant two-way communication.
In neurology, this connection – known as the gut-brain axis – is gaining attention for its role in brain health. Researchers are discovering that the state of your gut might influence conditions like brain inflammation, multiple sclerosis (MS), and even dementia.
A comprehensive brain health evaluation can help establish your cognitive baseline and monitor brain health over time. The good news is that by nurturing your gut health, you may also support your brain.
The Gut-Brain Partnership
The idea that caring for your gut can benefit your brain is an exciting development in neurology. While the science continues to grow, you can already start embracing a gut-healthy lifestyle.
Think of it as tending a garden: by feeding and caring for the "good" bacteria inside you, you're helping to protect your most vital organ – your brain. A happier gut just might lead to a healthier, brighter mind!
In this article, we'll explain the gut-brain axis in simple terms, highlight recent research on its role in neurological conditions, and give you practical tips to improve your gut-brain health with diet and lifestyle changes.
What is the Gut-Brain Axis?
The gut and brain communicate through nerves, hormones and chemicals, and immune signals. The vagus nerve (a large nerve connecting the brain and digestive tract) is a key pathway for this gut-brain communication, alongside chemical messengers that travel through the bloodstream. This two-way network is often called the gut-brain axis, linking digestive health and brain function.
| Component | Description |
|---|---|
| Major Nerves | The vagus nerve is a major nerve that connects the brain and digestive system. |
| Hormones and Chemicals | Hormones like serotonin and chemicals like microbial metabolites can travel between the gut and brain. |
| Immune System | The immune system can send signals between the gut and brain. |
The Vagus Nerve: Your Gut-Brain Communication Highway
At its core, the gut-brain axis is the constant dialogue between your digestive system and your nervous system. The brain sends signals to the gut and vice versa. One major player is the vagus nerve, a long nerve that runs from the brain to the abdomen, acting like a communication highway between the two organs.
Chemical Signals: Your Gut's Hidden Language
But communication isn't just through nerves – it also happens via chemical signals. Trillions of microbes in our gastrointestinal tract produce substances (including some of the same neurotransmitters our brains use) that enter the bloodstream and can affect the brain. In fact, about 90% of the body's serotonin – a neurotransmitter known for stabilizing mood – is made in the gut. No wonder scientists nickname our gut the "second brain," since it has its own extensive nerve network (over hundreds of millions of nerve cells!) and makes many brain-like chemicals.
Surprising Fact
Your gut contains hundreds of millions of nerve cells! This extensive neural network is why scientists often refer to the gut as your "second brain." This helps explain why your emotions can affect digestion and why gut health may influence mood and cognition.
The Connection: A Two-Way Street
This means that what happens in the gut doesn't stay in the gut. If you're stressed or anxious, your brain can send signals that upset your stomach (think of that nervous belly before a public speech). Conversely, an irritated gut can send signals that affect your mood and mindset. This intimate connection explains why gut health is increasingly viewed as vital to overall neurological well-being.
Gut Health and Neuroinflammation: The Fire Within
One of the most important ways the gut-brain axis affects neurological health is through the immune system and inflammation. Neuroinflammation refers to inflammation in the brain or spinal cord – essentially, an overactivation of the brain's immune responses. Many neurological disorders (like MS, Alzheimer's disease, and Parkinson's) involve chronic neuroinflammation. So what does the gut have to do with it?
A healthy gut acts as a barrier and an immune educator: the beneficial bacteria in your gut help maintain a balanced immune response. But an imbalanced gut (sometimes called gut dysbiosis) or a "leaky" gut lining can let inflammatory molecules into your bloodstream, triggering body-wide inflammation that may reach the brain.
Recent studies suggest that gut microbes can indeed modulate inflammation in the nervous system. For example, certain bacteria in the gut produce substances that can travel to the brain or stimulate immune cells, potentially increasing or decreasing neuroinflammation.
Signs of Poor Gut Health
Be aware of these potential indicators of gut imbalance that might affect your neurological health:
- Chronic digestive issues (bloating, gas, diarrhea, constipation)
- Unexplained fatigue or brain fog
- Food sensitivities or intolerances
- Frequent infections or autoimmune issues
- Unexpected mood changes or anxiety
If you experience these symptoms persistently, consider discussing gut health with your healthcare provider.
Researchers are finding links between gut health and the hallmarks of neurodegenerative diseases. In Alzheimer's disease, for instance, inflammatory molecules from the gut might encourage the buildup of amyloid plaques in the brain. In general, an unhealthy gut microbiome may prime the body for stronger inflammatory reactions, whereas a balanced microbiome can produce anti-inflammatory compounds. This connection is leading scientists to explore whether calming gut-related inflammation could help treat or prevent some neurological conditions.
The Gut-Brain Connection in Multiple Sclerosis (MS): A Promising Discovery
Multiple sclerosis is a prime example of a neurological disease where the gut-brain axis is under intense study. MS is a chronic inflammatory condition in which the immune system mistakenly attacks the protective coating of nerve fibers (myelin) in the central nervous system. Traditionally, MS has been managed by targeting the immune system, but emerging research points to the gut as a potential key factor in the disease's development and progression.
The MS - Microbial Connection
Studies have found that people with MS often have a different mix of gut bacteria compared to people without MS. In fact, the human gut microbiome (the collection of microbes in our intestines) produces thousands of metabolites and signals that communicate with the brain and immune system, and imbalances in these gut microbes have been linked to MS. Scientists have observed that certain beneficial bacteria tend to be fewer in MS patients, while some potentially inflammatory bacteria are more abundant. These microbial differences could influence how the immune system behaves. For example, gut bacteria can produce small molecules that might either dial down or ramp up inflammation throughout the body.
For MS Patients
If you have multiple sclerosis, consider these gut-friendly approaches alongside your medical treatment:
- Work with your neurologist on an anti-inflammatory diet plan
- Consider Mediterranean style diet, which has shown to have benefits in some MS studies
- Stay hydrated and maintain regular physical activity as tolerated
- Discuss probiotic options with your healthcare provider
- Track your symptoms in relation to diet changes
Remember: Dietary changes should complement, not replace, your prescribed MS treatments.
Evidence suggests that the gut microbiota can even trigger processes that worsen MS. Research in 2023 noted that gut microbes may promote oxidative stress (a type of cell damage) and inflammation in the brain, contributing to the neurodegeneration seen in MS.
This has exciting implications: if gut microbes are helping drive MS inflammation, could adjusting the gut microbiome help treat MS? Early findings say possibly yes. Growing evidence suggests that targeting gut bacteria could be a promising strategy for MS management. In experimental models, introducing "good" bacteria (probiotics) or even transplanting a healthy microbiome into animals can reduce MS-like symptoms. Clinical trials are now exploring diets and probiotic supplements to see if improving gut health might calm the MS immune attacks. While it's too soon to replace standard MS treatments with gut-focused therapy, MS patients are encouraged to maintain a healthy diet and lifestyle for overall wellness – and their gut may thank them for it.
The Gut-Brain Connection in Dementia: Memory and Microbes
Another area of intense research is how the gut might influence dementia, particularly Alzheimer's disease (the most common form of dementia). Alzheimer's is characterized by memory loss and cognitive decline, along with physical changes in the brain such as amyloid-beta plaques and tau tangles, often accompanied by brain inflammation. Scientists now suspect that the gut-brain axis may play a role in these changes.
How Could Gut Bacteria Affect the Brain of Someone with Dementia?
How could gut bacteria affect the brain of someone with dementia? One theory is through inflammation and toxic proteins. Harmful gut microbes can produce substances that can trigger strong immune reactions. If too much bacterial products enter the bloodstream (for example, due to increased gut permeability), they might reach the brain and activate immune cells there, promoting inflammation. Recent studies have indeed found that intestinal microbiota can influence neuroinflammation which in turn affects amyloid plaque formation in the brain. In simpler terms, an imbalance in gut bacteria might make the brain more inflamed and prone to the kind of damage seen in Alzheimer's disease.
Dementia Risk Factors You Can Control
While some dementia risk factors can't be changed, these gut-related factors are within your control:
- Diet high in processed foods and sugars (associated with increased risk)
- Chronic stress (damages both gut and brain health)
- Sedentary lifestyle (reduces beneficial gut bacteria diversity)
- Poor sleep habits (disrupts gut microbiome balance)
- Excessive alcohol consumption (harms gut barrier function)
Taking action on these factors may help protect both your gut and brain health as you age.
Gut Bacteria and Alzheimer's: Emerging Connections
Additionally, researchers have observed that patients with Alzheimer's often have a different gut microbiome profile than healthy older adults. Certain anti-inflammatory gut bacteria might be reduced, while others that produce inflammatory or harmful metabolites are increased. It's a correlational finding (meaning we don't know if one causes the other yet), but it opens the door to new possibilities. Could adjusting the gut slow down or change the course of dementia? Early experiments suggest it's worth investigating.
Of course, dementia is complex and multifactorial – gut health is likely just one piece of the puzzle. Nonetheless, maintaining a healthy gut environment could be a simple, proactive step to support brain health as we age.
Practical Tips for a Healthy Gut-Brain Connection
The connection between gut and brain means that taking care of one can benefit the other. Researchers often say, "what's good for the gut is good for the brain." While we await more discoveries, there are practical steps you can take now to improve your gut-brain health. Here are some tips backed by emerging research and medical experts:
Foods to Boost Gut-Brain Health
Yogurt with fruit is a gut-friendly choice. Fermented foods like yogurt provide beneficial bacteria (probiotics), while fruits such as bananas and berries offer prebiotic fiber to feed those good bacteria. Including such foods in your diet can help nourish your gut microbiome, which in turn may have positive effects on brain health.
Other gut-brain supporting foods include:
- Leafy greens (spinach, kale)
- Fatty fish rich in omega-3s (salmon, mackerel)
- Nuts and seeds
- Olive oil
- Colorful vegetables with diverse phytonutrients
Eat a plant-rich, high-fiber diet: Fuel Your Microbiome
Your gut microbes thrive on fiber and diverse natural foods. Aim to eat plenty of vegetables, fruits, whole grains, legumes, nuts and seeds. More variety in your diet leads to a more diverse gut microbiome, which is great for gut health. Fiber essentially acts as a prebiotic – food for beneficial bacteria – helping them produce brain-friendly nutrients. Also include probiotic-rich fermented foods like yogurt, kefir, kombucha, sauerkraut, or kimchi which can introduce helpful bacteria to your gut. Studies have found that diets high in fiber and fermented foods are linked to lower inflammation and even better mood and cognition. On the flip side, try to limit processed and high-sugar foods. Excessive added sugars, artificial sweeteners, very fatty foods, and alcohol can harm the microbiome and increase inflammation. Moderation is key – for example, enjoy sweets or red meat occasionally rather than daily.
The 3-Day Gut Reset
If you want to kickstart your gut health journey, try this simple 3-day reset:
- Day 1: Eliminate processed foods, added sugars, and alcohol. Focus on whole foods only.
- Day 2: Add fermented foods (yogurt, kombucha, sauerkraut) to each meal.
- Day 3: Include 30+ plant foods across the three days (vegetables, fruits, nuts, seeds, whole grains, legumes).
This quick reset can help reduce inflammation and begin rebalancing your gut microbiome.
Stay physically active: Move for Your Microbes
Regular exercise isn't just for your heart and muscles – it benefits your gut and brain too. Physical activity has been linked to a healthier diversity of gut bacteria and lower levels of inflammation. Aim for at least 150 minutes of moderate aerobic exercise per week (like brisk walking, cycling, or swimming), plus some strength training if you can. Exercise can directly reduce stress hormones and inflammation, which may create a healthier environment in both your intestines and your brain. Even a daily walk or gentle yoga can make a difference. Choose activities you enjoy so that you'll stick with them, and remember that moving your body regularly helps keep your digestion regular, your mood uplifted, and your brain sharp.
Manage stress and nurture mental well-being: Calm Mind, Happy Gut
Stress isn't just a state of mind – it has physical effects on your gut. High levels of chronic stress can alter your gut bacteria (often reducing the "good" kinds) and even increase gut permeability. Ever notice an upset stomach during times of anxiety? That's the gut-brain axis in action. To break the cycle, make stress management a priority. Simple practices like deep breathing, meditation, or progressive muscle relaxation can calm both brain and gut. Taking regular breaks to do things you enjoy – whether it's walking in nature, playing with a pet, or laughing at a funny video – can lower stress hormones and help rebalance your microbiome. Connecting with friends or a support group can also improve mental well-being (and healthy social interaction has been linked to better gut health too!). If you struggle with anxiety or low mood, don't hesitate to talk to a healthcare provider; improving your mental health is good for your gut health, and vice versa.
The Stress-Gut Connection
Research shows that chronic stress can damage your gut barrier within hours, allowing inflammatory substances to leak into your bloodstream. This "leaky gut" can trigger systemic inflammation affecting brain health.
Two effective stress-reduction techniques with research backing:
- Box breathing: Inhale for 4 counts, hold for 4, exhale for 4, hold for 4, repeat
- 5-minute nature exposure: Even brief time looking at trees or natural settings can lower stress hormones
Get enough sleep: Rest for Restoration
Sleep is when the body and brain repair themselves – and that extends to your gut. Persistent sleep deprivation can disrupt the gut microbiome and has been associated with increased inflammation and even heart and brain issues. Most adults need around 7–8 hours of quality sleep per night. To improve sleep quality, maintain a consistent bedtime schedule, create a dark and quiet bedroom environment, and avoid heavy meals or screen time right before bed. Better sleep will help regulate stress and appetite hormones, which in turn keeps your gut bacteria in balance and supports cognitive function.
By following these lifestyle tips, you create an environment in which your "good" gut bacteria flourish and communicate positive signals to your brain. Remember that changes won't happen overnight – the microbiome can take time to adjust – but over weeks and months, a healthier diet and lifestyle can meaningfully strengthen your gut-brain axis.
Summary and Key Takeaways: Your Action Plan for Gut-Brain Health
In summary, the gut-brain axis is a powerful illustration of how connected our bodies are. New neurology patients and anyone interested in brain health should be aware of this emerging science. Here are the key points to remember:
Your gut and brain are deeply connected. They constantly send messages back and forth through nerves (like the vagus nerve), chemical messengers, and immune system signals. This is why emotional stress can upset your stomach, and gut troubles can affect your mood. The trillions of microbes in your gut play a major role in this conversation, producing neurotransmitters and other chemicals that affect the brain.
Gut health influences brain inflammation and disease. An imbalanced gut microbiome can contribute to neuroinflammation – the kind of inflammation implicated in conditions like MS and Alzheimer's. Research has linked gut bacteria imbalances to autoimmune flare-ups in multiple sclerosis and to the progression of dementia. While we are still uncovering the exact mechanisms, it's clear that a healthy gut supports a healthier brain.
Emerging research offers hope. Scientists are exploring therapies that target the gut-brain axis – from probiotics and special diets to fecal microbiota transplants – as potential ways to treat neurological diseases. Early studies are promising (for example, probiotic supplements showed improved cognitive scores in Alzheimer's patients, and trials in MS are ongoing), but more research is needed. In the meantime, neurologists recognize the gut-brain link as an important piece of the holistic care puzzle.
You can take action through diet and lifestyle. Perhaps the most empowering lesson is that everyday habits matter. Eating a fiber-rich, plant-focused diet and including fermented foods can nurture your gut's beneficial bacteria. Managing stress, getting regular exercise, and sleeping well all support a healthy gut-brain axis. These changes not only improve digestion – they can boost your mood, sharpen your thinking, and reduce inflammation in your body.
Talk to your healthcare provider. Always let your neurologist or primary doctor know about any significant dietary changes or supplements (like probiotics) you're considering. They can offer guidance tailored to your situation. Remember that gut health is just one aspect of neurological care – it complements but doesn't replace traditional treatments. A balanced approach is best.
Start Today: Five Simple Steps
Begin your gut-brain health journey with these five steps anyone can take:
- Add one fermented food to your daily diet (yogurt, kimchi, etc.)
- Replace one processed snack with a fiber-rich alternative (fruit, nuts, vegetables)
- Take a 10-minute walk after meals to aid digestion and reduce stress
- Practice 5 minutes of deep breathing or meditation daily
- Set a consistent sleep schedule, aiming for 7-8 hours nightly
Small, consistent changes often lead to the most sustainable health improvements.
Learn More About Our Approach
Explore our comprehensive approach to neurological care at Achilles Neurology Clinic.
Book a Consultation
Schedule your consultation with our expert neurologists in Los Angeles.
About the Author
Dr. Achillefs Ntranos MD
Board-Certified Neurologist
Achilles Neurology Clinic
Dr. Achillefs Ntranos MD is a board-certified neurologist and MS specialist known for his thorough evaluations and compassionate approach. Originally from Greece, he trained at Johns Hopkins University and Mount Sinai Hospital before founding Achilles Neurology Clinic in Beverly Hills to deliver comprehensive, patient-centered neurological care. He specializes in MS, autoimmune neurology, neuropathy, headaches, and other neurological disorders, blending research-driven insights with personalized treatment plans.
References:
- Probiotics may help boost mood and cognitive function - Harvard Health
- What Is the Gut-Brain Connection? - Cleveland Clinic
- Beyond the brain: The gut microbiome and Alzheimer's disease - NIA
- Emerging role of gut microbiota dysbiosis in neuroinflammation and neurodegeneration - Frontiers
- The role of the gut microbiota in multiple sclerosis - News Medical
- The Gut–Brain Axis as a Therapeutic Target in Multiple Sclerosis - PMC
- Bacterial neurotoxic metabolites in multiple sclerosis cerebrospinal fluid and plasma - Brain